FAQ: CMS Rural Health Transformation Program

In October 2025, HIMSS hosted three office hour sessions to provide guidance on the Rural Health Transformation Program (RHTP) and to suggest resources and digital health model practices in support of state’s program applications. HIMSS policy and informatics experts answered attendee questions and shared insights relating to the tech innovation goals of the Centers for Medicare and Medicaid Services RHTP cooperative agreement with states.
As authorized by the One Big Beautiful Bill Act, the Rural Health Transformation Program will make $50 billion available to states to support health transformation activities in state programs and rural health hospitals and providers. States must apply for program funding by Nov. 5, 2025.
For more information, contact:
- Valerie Rogers, Senior Director, Government Relations Valerie.Rogers@himss.org
- Evan Dunne, Manager, Government Relations Evan.Dunne@himss.org
Office Hours FAQs & Important Notes
-
How much can States budget for tech innovation or digital health projects under the RHTP?
CMS is instructing States to develop a budget narrative as a part of their application for illustrative purposes, budgeting $200 million per year over five years across the States' proposed initiatives.
- States' budgets should reflect "best estimates" of the cost to operate each proposed initiative, and States will have the opportunity to revise them in their annual reports to CMS. Actual award amounts may be larger or smaller than $200 million per year based on CMS's review of applications.
- The sheer number of projects does not cap tech innovation projects under the Rural Health Transformation Program (RHTP). Still, there are specific financial caps and limitations on certain types of technology-related expenditures and on overall funding distribution.
- Ex. CMS places a 5% cap on replacing HITECH-certified electronic health records (EHRs), so States are likely to focus on enhancements or add-ons (including AI-enabled tools) rather than wholesale system overhauls. Comprehensive AI integration may require newer platforms.
- CMS allows upgrades, enhancements, and the addition of modules, interfaces, or functionality to existing EMR/EHR systems as allowable uses of funds and are not subject to the 5% limitation. Furthermore, providers may substitute G10-certified modules to meet their needs, and this substitution is not subject to the 5% limitation. These upgrades, enhancements, and additions of modules, interfaces, or functionality to existing EMR systems should be aligned with CMS's Health Technology Ecosystem criteria (including the CMS Interoperability Framework) and ASTP/ONC criteria, as applicable to the contemplated use of funds.
- G10 is a critical compliance requirement under the 21st Century Cures Act Final Rule, issued by the Office of the National Coordinator for Health IT (ONC). It mandates that certified health IT systems expose FHIR R4-based APIs using SMART on FHIR protocols, enabling secure, standards-based access to patient and population health data.
-
Can RHTP funds be used to develop a health information exchange or advance Community Information Exchange (CIE)?
Yes! Rural Health Transformation Program (RHTP) funds can be used to develop a health information exchange. The RHTP encourages technological innovation and includes provisions for activities that support and strengthen health information exchange capabilities in rural areas. According to CMS, Specific eligible uses that support health information exchange include:
- Investing in technology, telehealth, and cybersecurity: Funds can be used for software, hardware, and technical assistance for "significant information technology advances" designed to improve efficiency, enhance data security, and improve patient health outcomes.
- Improving data sharing: One of the program's goals under "Tech innovation" is to foster innovative technologies that "support access to remote care, improve data sharing, strengthen cybersecurity, and invest in emerging technologies."
- Strengthening connectivity and interoperability: The program is a chance to "strengthen connectivity”, improve interoperability, and ensure that rural patients are not left behind in the digital health era. Better data exchange means safer care, stronger outcomes, and more equitable access."
- Developing standards-based platforms: Funds can be used for the development of platforms that integrate and store patient health data from various sources (e.g., remote monitoring devices and existing health records), enabling seamless exchange.
-
Can RHTP funds be used for an EHR system?
Yes, Rural Health Transformation Program (RHTP) funds can be used for an EHR system, but there are some limitations.
The funds are intended for "significant information technology advances" and "EHR upgrades," but not for replacing a system that is already fully functional and HITECH-certified. Further, CMS has outlined some restrictions related to EHR/EMR systems:
- Replacement of Existing HITECH-certified Systems: No more than 5% of the total RHTP funding awarded to a state in each budget period may support the replacement of an existing HITECH-certified EMR system that was in place as of September 1, 2025.
- Clinical Services Reimbursement: Funds cannot be used to replace payments for clinical services already reimbursable by Medicaid, Medicare, or other federal programs.
-
To what degree are connected dx utilized in any applications? For example, at-home testing and data capture (a visual image capture) of a test result. Can Dx be used as part of clinical workflows and telehealth for remote care delivery?
Connected diagnostic (Dx) technologies are increasingly integrated into programs like the CMS RHTP (Remote Health Testing Program) to enhance remote care delivery.
- An example use case for the RHTP may include home-based diabetes or hypertension monitoring devices that transmit data automatically.
- CMS has shown increasing support for telehealth and remote diagnostics, including reimbursement policies for remote monitoring, which encourages broader adoption.
- HIMSS will follow the RHTP program to identify states where Dx is incorporated in the state plans. However, the trend is toward significant growth in reliance on connected Dx tools, especially for visual imaging and digital reporting.
-
The application discusses the Rural Tech Catalyst Fund Initiative (see appendix, page 115). Does HIMSS have any additional details about this or an overview of how other States or CMS may be thinking about this? It appears that up to 20M a year can be directed to supporting innovation and startup initiatives focused on solving complex rural health issues.
The Rural Tech Catalyst Fund Initiative is a component of the Rural Health Transformation Program (RHTP) that specifically directs funds towards technology and digital health projects to improve rural healthcare access, efficiency, and quality, and to encourage the development and adoption of consumer-facing, technology-driven solutions for prevention and chronic disease management in rural populations.
- Focus: Primarily on advancing technology, innovation, or broadband connectivity in rural areas.
- Goals: To support rural communities in adopting new technologies, improving digital infrastructure, and fostering innovative ecosystems.
- Activities: Funding for technology startups, infrastructure projects, digital skills training, and other initiatives aimed at bridging the digital divide in rural regions. CMS also encourages technology-driven solutions (including those that support evidence-based, measurable interventions) for prevention and management of chronic diseases where traditional government funding sources and private commercial incentives have proven inadequate or insufficient to drive development and innovation.
- Funding for the "catalyst fund" is capped at the lesser of 10% of a state's total RHTP award (up to $200 million/yr can be budgeted) or $20 million per budget period.
- States should consider addressing how data will flow across health systems, pharmacies, and state agencies (interoperability, consent, eligibility engines), and any digital health infrastructure needs could be resolved, thus ensuring that every rural resident can access tech-enabled care through the use of the "catalyst fund."
-
The NOFO workforce development section seems specifically focused on expanding access to clinicians in rural areas. Could it also support workforce needs within the public health organization?
According to CMS, States may also sub-award or contract RHTP funds to eligible partners, such as universities, local health departments, and provider associations, to carry out approved activities. Therefore, public health and community health (CHWs) workforce needs can be addressed through the RHTP, and it is encouraged to improve rural health outcomes.
- Specifically, consider how public health, community health, Medicaid, and behavioral health workers can support the initiative's primary aims and extend providers' reach.
- Professional Development: Providing funds for ongoing professional development, training, and certification for the existing workforce, including support for supervisors of CHWs and other extenders that may include public health specialists.
- Further, the RHTP funding allows for investment in health information technology (IT) and technical assistance, which can alleviate workforce burdens and improve efficiency:
- Telehealth and Remote Monitoring: Implementing telehealth platforms and remote patient monitoring systems, enabling providers to expand access to care and reduce unnecessary hospital admissions.
- Efficiency-Enhancing Technology: Providing software and hardware for IT advances that improve workflow efficiency and reduce provider burnout. AI and other enterprise solutions can help coordinate care and reduce administrative burden.
-
What role will policymakers play in the planning and implementation of the RHTP?
CMS requires the Governor's office to submit the state's RHTP application, along with a letter of endorsement and a commitment to aligning health and economic policies to ensure the program's success.
- Note, States must submit descriptions of current state policy — and CMS may reward States that shape future legislative or regulatory action—across a disparate list of policy domains, including state telehealth laws, scope-of-practice regulations, etc.
- Further, the National Conference of State Legislators (NCSL) identified several examples in which state legislators have either introduced (North Carolina and Pennsylvania) or enacted (California, Michigan, and Utah) legislation addressing the Rural Health Transformation Program. Most of these bills establish a dedicated fund for the RHTP once it is awarded and distributed, or they provide the necessary approvals for state agencies to receive large federal awards.
For more information about the NOFO and the program, visit the Centers for Medicare and Medicaid Services (CMS) updated frequently asked questions document and a scoring fact sheet for the Rural Health Transformation Program (RHTP).
The scoring fact sheet provides the scoring calculation steps for workload funding as well as an example of how state scores translate to funding amounts.
HIMSS Resources and Tools
AI and Predictive Analytics continue to dominate conversations and budgets. But the shift is toward targeted, clinical use cases: triage, diagnostics, care coordination, and population health management. Payers and providers are looking for platforms that not only predict but also act, improving workflows and outcomes simultaneously. HIMSS offers the Analytics Maturity Assessment Model (AMAM), assisting health systems in refining data governance and analytics strategies, thereby facilitating effective and equitable AI adoption.
Virtual Care Platforms have matured beyond basic telehealth. Hybrid care models, remote monitoring, and asynchronous communication tools are gaining traction. The winners in this space are focused on clinical integration and reimbursement alignment, not just convenience. Join the HIMSS Virtual Care Community of Practice to learn more.
Digital Therapeutics are seeing renewed interest, particularly in behavioral health, chronic condition management, and oncology. As regulatory clarity improves and evidence bases grow, investors are watching closely. Visit HIMSSTV Digital Therapeutics Alliance Summit for case-based examples.
HIMSS Davies Award of Excellence showcases model practices supporting improvements in rural health outcomes and the successful management of chronic diseases.
HIMSS Digital Health Indicator and Maturity Models are tools that can support the Rural Tech Catalyst Fund Initiative, a call to action for tech innovation included in the RHTP.
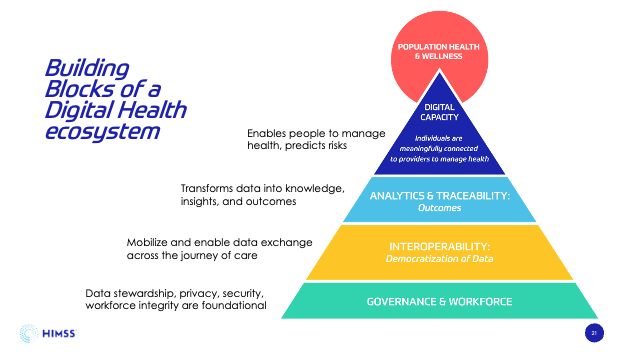
HIMSS encourages every state to utilize the Digital Health Indicator and maturity models to advance and sustain rural digital health adoption.
These tools can help states:
- Establish a nimble, rapid-cycle learning health system environment (analytics, strategic coordination)
- Advance the coordination of easy, trusted, and secure access to multi-modal health data across virtual, remote, or in-person services.
- Ensure the public can access virtual and remote services, including high-speed broadband and ongoing reimbursement of virtual health services across the spectrum of care, and accelerate digital health literacy.
- Modernize the chronic disease data systems to ensure a comprehensive approach to value-based whole-person care and population health.
An excellent resource demonstrating the value of these tools to improve digital health capacity in rural environments is the Missouri Dept of Health and Senior Services DHI project, which can be used as a guide to help your state launch a similar project.
See: Summary of DHI project in Missouri and full report. To learn more, please reach out to Alana Lerer (alana.lerer@himss.org) and Toby Bazarnick (toby.bazarnick@himss.org).
Rural Health Model practices and HIMSS TV Highlights
- Using AI to Address Multiple Chronic Conditions in Rural Environments: AI snapshots tailored to rural health challenges
- Robust EMR Systems Ensuring Quality of Care in Rural Areas using HIMSS Maturity Models:
HIMSS Informatics and Policy Staff Contacts
Would you be interested in learning more about HIMSS Digital Health Transformation Solutions? Please reach out to:
- Alana Lerer, Senior Government Relations Manager, Alana.Lerer@himss.org
- Toby Bazarnick, Vice President Provider Sales, Toby.Bazarnick@himss.org
Public Policy and Model Practices:
- Valerie Rogers, Senior Director, Government Relations and Valerie.Rogers@himss.org
- Evan Dunne, Manager, Government Relations (Tribal Health, Chapter Advocacy) Evan.Dunne@himss.org
Clinical Informatics and Artificial Intelligence:
- Whende Carroll, Clinical Informatics Advisor, Whende.Carroll@himss.org
- Gwynne Jelbaoui, Senior Program Manager, Clinical Informatics, gwynne.jelbaoui@himss.org
Learn more information about HIMSS's efforts to bridge healthcare and public health through the power of digital health transformation.
-
HIMSS Public Policy and Advocacy
At HIMSS, we educate, conduct research and offer strategic public policy recommendations, driving digital health transformation to realize the full health potential of every human everywhere.